Introduction
Modern dentistry is witnessing a quiet revolution — one that aims not just to repair teeth but to regenerate them.
The Regenerative Endodontic Procedure (REP), sometimes called regenerative pulp therapy, represents a major leap in dental science. Unlike traditional root canal therapy that removes all the infected tissue, REP focuses on healing, regeneration, and restoration of the tooth’s natural vitality.
This advanced approach is transforming how dentists handle immature or non-vital teeth, especially in younger patients. But the benefits go beyond age — the principles of regeneration could redefine the future of painless, biologically centered dental care.
In this post, we’ll explore what REP is, how it works, its scientific foundation, benefits, and what the future holds for regenerative endodontics.
What Is a Regenerative Endodontic Procedure (REP)?
A Regenerative Endodontic Procedure is a biologically based treatment designed to replace damaged pulp tissue (the soft core of the tooth) with new, living tissue.
It stimulates the body’s natural healing ability to restore root development, dentin formation, and in some cases, pulp vitality.
In simple terms, REP doesn’t just “fill” the root canal — it revives it.
This treatment is particularly effective for:
- Immature permanent teeth with incomplete root development
- Teeth with pulp necrosis (dead pulp) due to trauma or infection
- Teeth requiring revitalization rather than replacement
The ultimate goal of REP is to promote continued root growth, thicken dentinal walls, and strengthen the tooth structure naturally.
The Science Behind REP
REP is grounded in the principles of tissue engineering, which involves three essential elements:
- Stem cells – the body’s natural building blocks for regeneration
- Growth factors and signaling molecules – to stimulate cell differentiation
- Scaffold – a 3D framework (often made from blood clots or biomaterials) that supports cell growth
In REP, the dentist triggers bleeding into the cleaned root canal to form a blood clot scaffold that contains stem cells. These stem cells, primarily from the apical papilla, migrate into the root canal and start forming new tissue — dentin, blood vessels, and sometimes even nerve fibers.
According to the American Association of Endodontists (AAE), REP promotes the regrowth of functional pulp-like tissue, not just sterile filling.
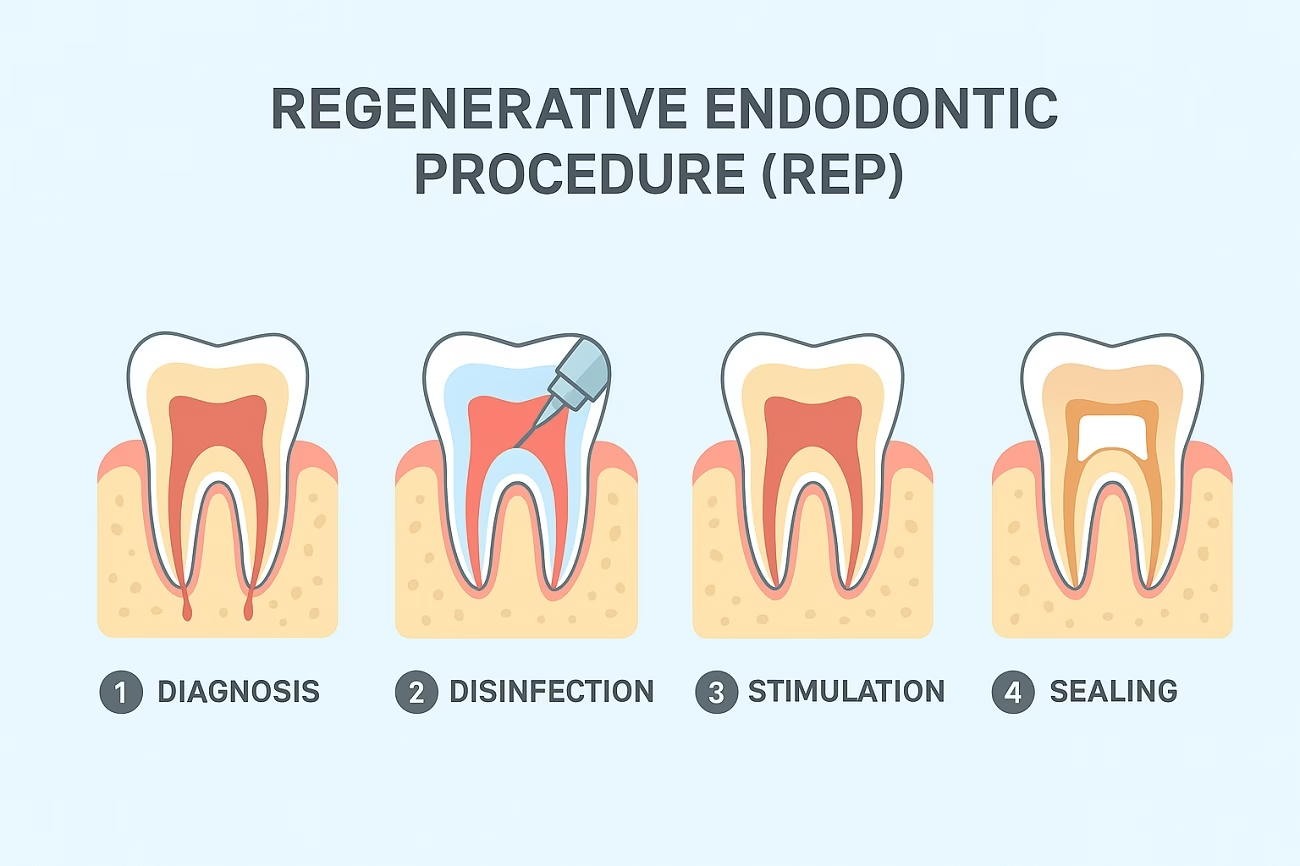
Step-by-Step: How REP Is Performed
The regenerative endodontic procedure typically unfolds over two visits, following a careful biological protocol.
Step 1: Diagnosis and Case Selection
The dentist evaluates the tooth’s condition using X-rays and pulp vitality tests. REP is usually chosen when the tooth is immature and the root apex is open, providing room for blood flow and healing.
Step 2: Canal Disinfection
Instead of aggressive mechanical cleaning, minimal instrumentation is used to preserve the remaining healthy tissue.
The canal is disinfected using gentle irrigants like sodium hypochlorite (NaOCl) and EDTA, which remove bacteria while preserving stem cell viability.
Step 3: Intracanal Medication
A medicated paste — commonly triple antibiotic paste (ciprofloxacin, metronidazole, minocycline) or calcium hydroxide — is placed inside the canal for 1–4 weeks to eliminate infection.
Step 4: Inducing Bleeding
At the second visit, the dentist removes the medicament and carefully irritates the apical tissue with a sterile file to induce controlled bleeding into the canal space.
The blood clot acts as a natural scaffold, rich in stem cells and growth factors.
Step 5: Sealing the Tooth
Once bleeding reaches a suitable level (1–2 mm below the cementoenamel junction), a biocompatible material such as Mineral Trioxide Aggregate (MTA) or Biodentine is placed over it.
The tooth is then sealed permanently with a composite restoration.
Over time, this biologically rich environment allows new dentin and pulp-like tissue to form inside the root canal.
Key Benefits of Regenerative Endodontic Procedures
| Benefit | Description |
|---|---|
| Natural Healing | Encourages the body’s own stem cells to rebuild pulp and dentin. |
| Continued Root Growth | Especially in young patients, roots continue to lengthen and strengthen. |
| Increased Tooth Strength | Thickened dentinal walls make the tooth less prone to fracture. |
| Less Invasive | Minimal mechanical instrumentation compared to traditional root canals. |
| Biocompatible | Uses natural scaffolds and tissue-friendly materials. |
| Long-Term Viability | Potential to restore natural sensation and vitality in some cases. |
REP vs. Traditional Root Canal Treatment
| Feature | Traditional RCT | Regenerative Endodontic Procedure |
|---|---|---|
| Goal | Eliminate infection and fill canal with inert material | Regenerate pulp-like tissue and restore vitality |
| Approach | Mechanical cleaning and gutta-percha filling | Biological regeneration with stem cells |
| Indication | Mature, fully developed roots | Immature teeth with open apex |
| Outcome | Non-vital, functional tooth | Potentially vital, growing tooth |
| Follow-Up | No root development | Continued root growth and healing |
Scientific Evidence and Clinical Success
Numerous studies published in PubMed, Journal of Endodontics, and NIH reports have shown promising results for REP:
- Jeeruphan et al. (2012, JOE) demonstrated that REP resulted in greater root wall thickening and continued root development compared to apexification.
- American Association of Endodontists (AAE, 2021) established REP as a standardized biologically based procedure for immature necrotic teeth.
- Torabinejad & Faras (2012, JOE) noted that REP outcomes include resolution of periapical lesions and positive vitality tests in many cases.
These findings highlight REP’s potential to transform conventional endodontic outcomes from “replacement” to regeneration.
Who Can Benefit from REP?
REP is most suitable for:
- Children and adolescents with incompletely developed roots
- Patients with traumatic dental injuries causing pulp necrosis
- Cases where apexification has failed or is undesirable
- Teeth with wide apical openings
- Patients seeking biologically conservative treatments
However, REP is not ideal for:
- Fully mature teeth with closed apices
- Severe crown destruction with no remaining dentin
- Infected teeth without viable apical tissue
Your endodontist determines suitability after clinical and radiographic evaluation.
Materials Used in REP
| Category | Examples | Function |
|---|---|---|
| Irrigants | Sodium hypochlorite, EDTA | Disinfection while preserving stem cells |
| Intracanal Medicaments | Triple antibiotic paste, calcium hydroxide | Eliminates infection |
| Scaffold | Blood clot, platelet-rich plasma (PRP), platelet-rich fibrin (PRF) | Supports tissue growth |
| Biomaterials | MTA, Biodentine | Seals and promotes regeneration |
The Future of Regenerative Endodontics
The next generation of REP aims to use advanced stem cell biology, 3D bioprinting, and growth factor delivery systems to engineer fully functional pulp–dentin complexes.
Research is exploring:
- Scaffold-free cell therapy, allowing natural tissue formation
- Gene-activated matrices for enhanced healing
- Laser-assisted REP for better disinfection and precision
- Nanotechnology-based materials for improved sealing and regeneration
As biotechnology advances, REP may one day allow complete restoration of tooth vitality — including nerve and immune functions — marking a true biological cure for pulp disease.
Risks and Limitations
While promising, REP is still evolving. Limitations include:
- Variable outcomes depending on case selection and operator skill
- Tooth discoloration (especially with minocycline)
- Possible reinfection if coronal seal fails
- Uncertain long-term vitality in all cases
Nevertheless, the overall success rate remains high, with studies reporting over 80–90% positive outcomes in properly selected cases.
Patient Experience and Post-Care
After REP, patients may experience mild discomfort or sensitivity for a few days. Standard care includes:
- Avoiding hard foods until healing stabilizes
- Maintaining strict oral hygiene
- Follow-up radiographs every 6–12 months to monitor root growth
Most patients report no postoperative pain, and radiographs often show progressive root maturation over time.
FAQs
Q1. Is Regenerative Endodontic Procedure painful?
No. REP is performed under local anesthesia and is typically less invasive than a traditional root canal.
Q2. How long does REP take?
Usually two appointments spaced 2–4 weeks apart, depending on infection control.
Q3. Is REP suitable for adults?
Primarily for immature teeth, but new research suggests modified protocols for adults may work in selected cases.
Q4. Can the regenerated pulp feel temperature again?
In some successful cases, vitality tests show positive responses — indicating partial nerve regeneration.
Q5. What is the success rate?
Recent studies report over 85% clinical success, depending on technique and case selection.
Q6. How much does it cost?
REP costs more than conventional root canal treatment due to materials and precision but is still more affordable than implants or crowns.
Conclusion
The Regenerative Endodontic Procedure (REP) is not just a treatment — it’s a paradigm shift in dentistry.
It merges the science of stem cells, growth factors, and biomaterials to achieve something once thought impossible — regenerating a dead tooth.
As research progresses, REP may soon become a mainstream solution, offering millions of patients the opportunity to preserve their natural teeth for life.
This biologically inspired, minimally invasive approach represents the future of endodontics — where the goal is no longer to “fill canals” but to revive them.
Internal Links
External References:
- American Association of Endodontists – Regenerative Endodontics Guidelines
- PubMed Central – Regenerative Endodontic Therapy Studies